


womens health
Ectocervix - flat cells - squamous cell cervical cancer
Squamous cells - flat cells that look like fish scales. The word comes from Latin "squama" meaning "the scale of a fish or serpent". Our outer-layer skin cells are squamous cells, as well as the passages of the respiratory and digestive tracts, and the linings of hollow internal organs.
Endocervix - glandular cells - adenocarcinoma of the cervix
The endocervix is the inside of the cervix. There are glandular cells lining the endocervix; these cells produce mucus. These glandular cells can become cancerous, leading to adenocarcinoma of the cervix. Adenocarcinoma - any cancer that develops in the lining or inner surface of an organ.
Transformation zone
This is where cervical cells are most likely to become cancerous. The transformation zone is located around the opening of the cervix, leading on to the endocervical canal (narrow passageway running up the cervix into the uterus). During cervical screening doctors and nurses will focus on this area.
The symptoms of Cervical Cancer:
Cervical cancer is a silent killer. The biggest difficulty in cervical cancer is that it hardly shows any symptoms, not until it reaches a advanced stage, though it differs from woman to woman. The symptoms are often misinterpreted as PMS or Ovulation pains. That is why women should have regular cervical smear tests
The most common symptoms are: Bleeding between periods, Bleeding after sexual intercourse, Bleeding in post-menopausal women, Discomfort during sexual intercourse, Smelly vaginal discharge, Vaginal discharge tinged with blood, Pelvic pain

The causes of Cervical Cancer:
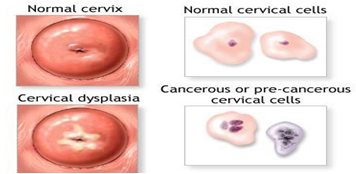
Cancer is the result of the uncontrolled division of abnormal cells. Most of the cells in our body have a set lifespan; when they die new cells are produced to replace them. Abnormal cells can have two problems: 1. They don't die. 2. They continue dividing. This results in an excessive accumulation of cells which eventually form a lump - a tumor. Scientists are not completely sure why cells become cancerous. However, there are some risk factors which are known to increase the risk of developing cervical cancer. These risk factors include:
HPV (Human Papilloma Virus)
Human papilloma virus infection is a sexually transmitted virus. There are over 100 different types of HPVs - 15 types can cause cervical cancer; probably 99% of them. In addition there are a number of types which can cause genital warts. It is estimated that HPV types 16 and 18 cause about 70% of cases cervical cancer while HPV types 6 and 11 cause 90% of genital warts. Other HPV types can cause cervical intra-epithelial neoplasia (CIN) - the growth of abnormal cells on the surface of the cervix.
Many sexual partners, becoming sexually active early
Socio-economic status.
Studies in several countries have revealed that women in deprived areas have significantly higher rates of cervical cancer, compared to women who live in other areas. Studies have also found higher rates in women of working age in manual jobs, compared to women in non-manual jobs. The most likely reason is a difference in the proportion of women who have regular screening.
Other main reasons are Smoking, Weakened immune system, Certain genetic factors, Long-term mental stress, Giving birth at a very young age, Several pregnancies, Long term use of Contraceptive pill, Other sexually transmitted diseases (STD).
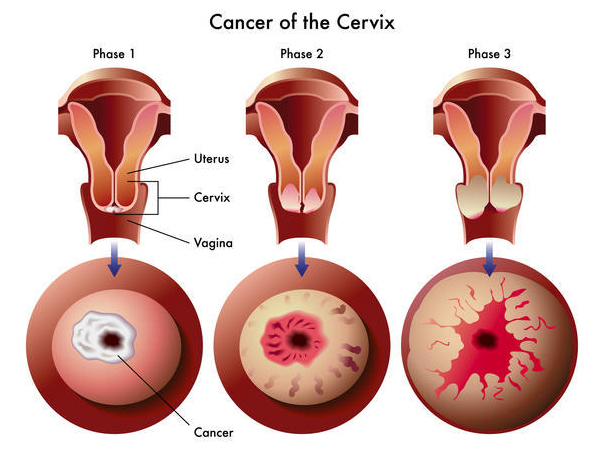
Cervical Cancer Diagnosis:
Cervical cancer being the third most common cancer in women of developing countries required improved early detection of the precursor’s lesions of cervix. This early detection helps in reducing the morbidity in women of these countries who are less educated and have poor access to medical treatment.It can be cured if it detected earlier. But the catastrophe is that the people will diagnose it only in the advanced state. The victims are often from the Socio-Economic Margins espcashewnut workers etc.
Cervical cancer occurs most commonly in women over the age of 30. According to the World Health Organization (WHO) at least 300,000 women worldwide die of cervical cancer each year.
WHO adds that if the HPV vaccine is administered globally, hundreds of thousands of lives each year could eventually be saved.Cervical cancer screening should occur no more than once every three to five years.
India Has Most Cervical Cancer Death
More women in India die from cervical cancer than in any other country, according to a new report that warns deaths from this preventable disease will rise unless attitudes to women change.
Cervical cancer kills around 72,000 women in India every year, more than 26% of the 275,000 deaths worldwide, says the report by the Cervical Cancer Free Coalition.
In India, maximum people die out of cervical cancer. According to the recent studies, it is proved that 130 female die out of cervical cancer per lakh population in 2013. According to the FDA [Federal Drug Authority] guidelines, any woman above 15 years should undergo the screening test if they had a sexual contact.
Cervical screening - LBC or Pap smear test
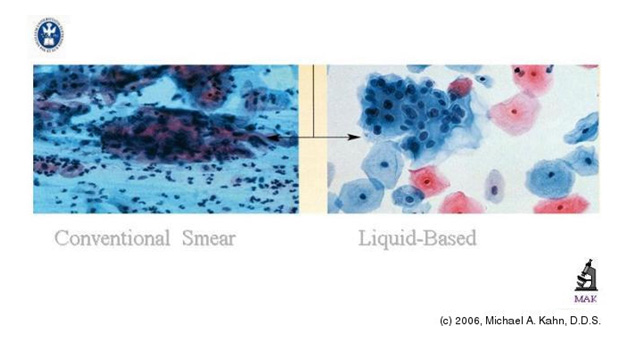
Cervical Screening used to be the old Pap smear Test - which is still used in many parts of the world. More recently, testing using LBC (liquid based cytology) has become more commonplace. A sample of cells is taken from the cervix. The doctor or nurse inserts a speculum - an instrument used to widen the opening of the vagina so that the cervix is more easily visible - and uses a spatula which is brushed around the cervix. The procedure is just mildly uncomfortable for the majority of women. If abnormal cells are there, there is a good chance they will be detected, but not always.
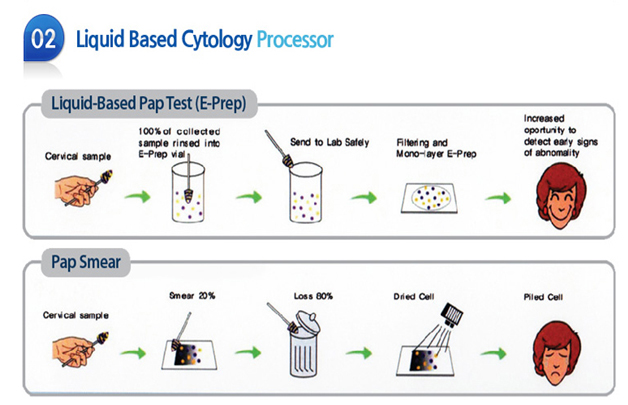
For many years, efforts have been made to develop methods that would enhance the sensitivity and specificity of the Papanicolaou smear (also called). Emphasis has been placed on creating automated screening machines whose success depends on a representative sampling of cells on standardized slides containing a monolayer of well-stained, well-preserved cells
From this research and development, liquid-based gynecologic specimen collection has evolved. Its proponents argue that liquid-based preparations outperform conventional smears because of improved fixation, decreased obscuring factors, and standardization of cell transfer. Proponents point out that, in direct smears, the cells are not transferred in a representative fashion and that up to 90% of the material scraped from the cervix may be discarded with the sampling device. With liquid-based collection, the sampling will be representative and operator-dependent variation will not occur since processing is controlled by the laboratory.
Introduction of LBC method helped to improve the diagnosis of precursor lesions of cervix
Liquid Based Cytology

However, the current technologies available today require sophisticated Instrumentation which makes the whole system expensive for a common set up to use this method routinely. Besides, the high cost of these patented, commercial systems required of cytotechnologists and pathologists in order to interpret the automated LBC slides, has led to the development and evolution of alternative, less costly methods.

With this regard bioDis has launched a Revolutionary Technology, a Liquid based Cytology which is Manually Processed named Citofem, approved by the U.S.Food and Drug Administration (FDA) for cervicovaginal testing. Preliminary evaluation showed the method to be as efficacious and, in two instances, more specific than its conventional smear counterpart.











